Endodontics is the dental specialty that deals with the nerves of the teeth. Root canals are probably the most notorious procedure in dentistry and the most common procedure relating to endodontics. When a tooth becomes infected it is usually related to the nerves in the root of the tooth. The infected nerves need to be removed. If left untreated an infection can turn into an abscess, which is a much more serious problem that includes bone loss in the jaw.
The area around the tooth is numbed with a local anesthetic to start the procedure. The dentist will then drill down into the tooth to create an opening into the canal. They will then be able to remove infected tissue and clean the canal. After the infection has been removed, the space is filled with a sealant called gutta percha. It is highly recommended that a tooth that has undergone a root canal is fitted with a crown. This will improve the structure and strength of the tooth, and increase the success rate of the root canal.
“Root canal” has become a scary term for dental patients to hear, but the benefits of the procedure and advances in dental technology have made it much less “scary”. Local anesthetics and proper pain medication allow the procedure to be performed with little to no pain in most cases. There may be some soreness following the procedure, but that is normal for most dental procedures. Over the counter painkillers are usually enough to relieve any pain afterwards, but your dentist may prescribe medication. The procedure will also relieve you from pain caused by the infection, allowing you to enjoy all the foods you love without any pain from heat, cold, or biting too hard. If you are experiencing pain, consult your dentist today.
Retreatment
With proper care, most teeth that have had endodontic (root canal) treatment can last as long as other natural teeth. Root canals performed by endodontists (root canal specialists) have a 95% success rate. In some cases, however, a tooth that has received endodontic treatment fails to heal. Occasionally, the tooth becomes painful or diseased months or even years after successful treatment.
Why do I need retreatment?
As occasionally happens with any dental or medical procedure, a tooth may not heal as expected after initial treatment for a variety of reasons:
- Narrow or curved canals were not treated during the initial procedure.
- Complicated canal anatomy went undetected in the first procedure.
- The placement of the crown or other restoration was delayed following the endodontic treatment.
- The restoration did not prevent salivary contamination to the inside of the tooth.
- In other cases, a new problem can jeopardize a tooth that was successfully treated.
For example:
New decay can expose the root canal filling material to bacteria, causing a new infection in the tooth. A loose, cracked or broken crown or filling can expose the tooth to a new infection. A tooth sustains a fracture. Retreatment is performed in two visits and involves the following:
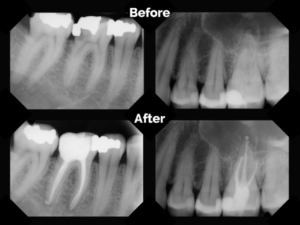
At the initial visit the endodontist will examine the tooth, take x-rays and discuss your treatment options. If you and your endodontist choose retreatment, the retreatment will be scheduled at that time for a future date.
- At the retreatment appointment the endodontist will administer local anesthetic to numb the tooth. After the tooth is numb, the endodontist will reopen your tooth to gain access to the root canal filling material. In many cases, complex restorative materials (crown, post and core material) must be disassembled and removed to permit access to the root canals.
- After removing the canal filling, the endodontist can clean the canals and carefully examine the inside of your tooth using a microscope, searching for any additional canals or unusual anatomy that requires treatment.
- After cleaning the canals, the endodontist will fill and seal the canals and place a temporary filling in the tooth. Post space may also be prepared at this time.
- After your endodontist completes retreatment, you will need to return to your dentist as soon as possible to have a new crown or other restoration placed on the tooth to protect and restore it to full function.
- If the canals are unusually narrow or blocked, your endodontist may recommend endodontic surgery.
Apicoectomy
An apicoectomy (endodontic surgery) is performed after an unsuccessful root canal. When an infection will not go away or returns after a root canal has been performed this procedure is usually necessary. There are many nerves that may contain the infected tissue, so it is difficult to ensure that all of the infection is removed during a root canal. During an apicoectomy, the tip of the root of the tooth is removed and replaced with a filling.
In most cases a second root canal is considered before an apicoectomy since it is a simpler, less invasive procedure.
Before the apicoectomy begins you will be given a local anesthetic to numb the area. The doctor will start by making an incision in your gum to expose the root of your tooth. Any inflamed tissue will be removed to clean out the area. The surgery takes place in a very small area, and only a few millimeters are removed from the root. For this reason, the doctor will use magnification and small precision instruments to perform the surgery. The precise nature of the surgery gives it a high rate of success. After the root is removed a filling is placed and the gums are sutured. Depending on the type of sutures you may have to return in a few days to have them removed, or dissolving sutures may be used instead. Over the course of the next few months the bone will heal around the root.

